7 Jabotinsky st. Moshe Aviv tower, 19th floor. Ramat-Gan
7 Jabotinsky st. Moshe Aviv tower, 19th floor. Ramat-Gan
Melanonychia refers to the darkening or pigmentation of the nail plate. It can be caused by various factors, including trauma, bacterial or fungal infections, systemic diseases, and benign or malignant conditions. This article focuses on the diagnosis and management of melanonychia, providing insights into the evaluation process and potential treatment options.
Diagnosing melanonychia involves a comprehensive evaluation of the patient’s medical history, physical examination, dermoscopy, and digital dermoscopy follow-up. The following steps are typically taken to determine the cause and appropriate management:
Medical history: The dermatologist gathers information about the patient’s general health, previous nail trauma or infections, medications, and family history of nail disorders or melanoma. This information helps identify potential triggers and risk factors.
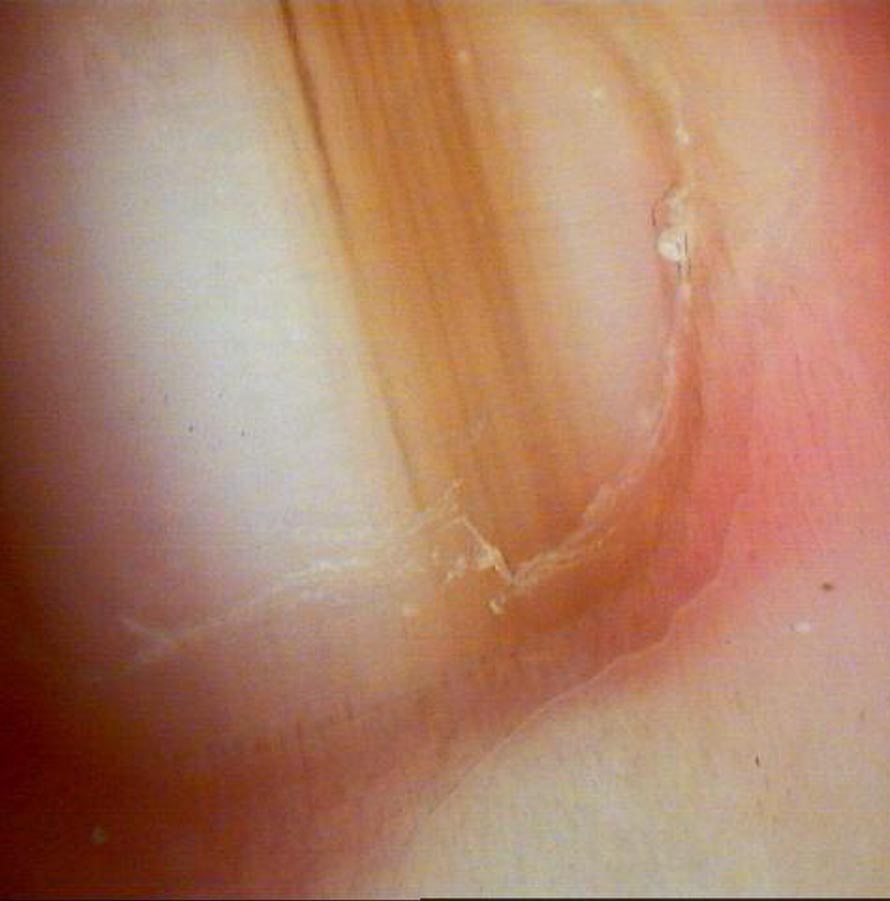
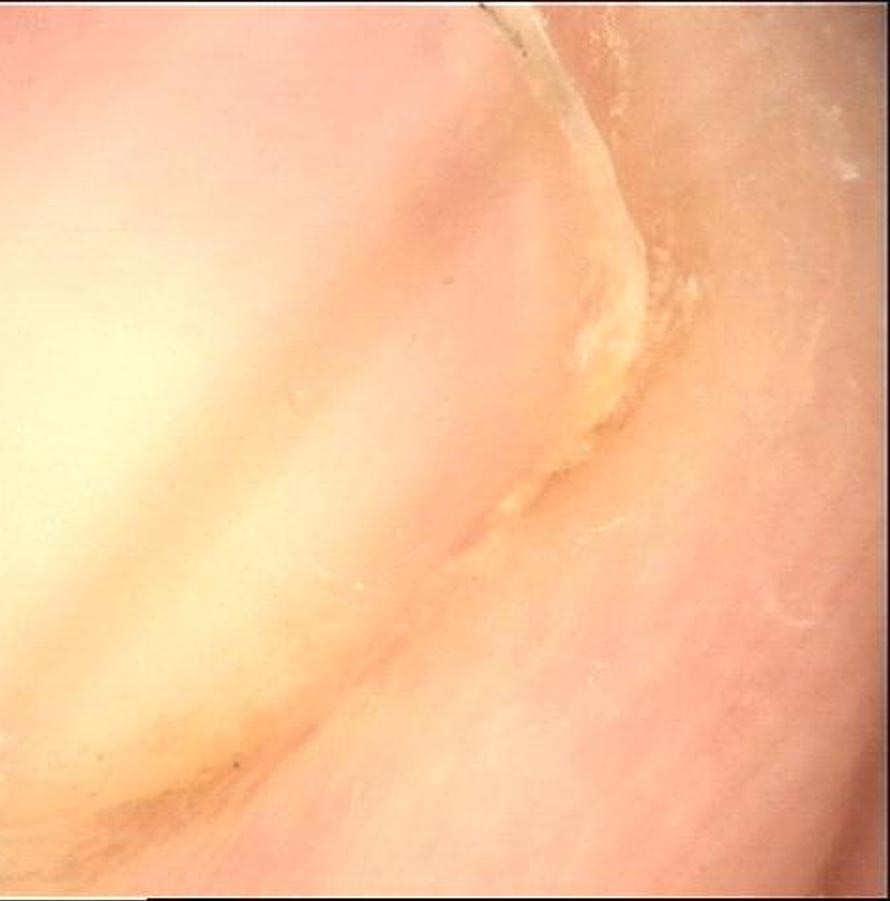
Physical examination: A thorough examination of the affected nail(s) is performed to assess the characteristics of melanonychia. This includes evaluating the pattern, width, and location of pigmentation, as well as examining the surrounding tissues for signs of inflammation or infection.
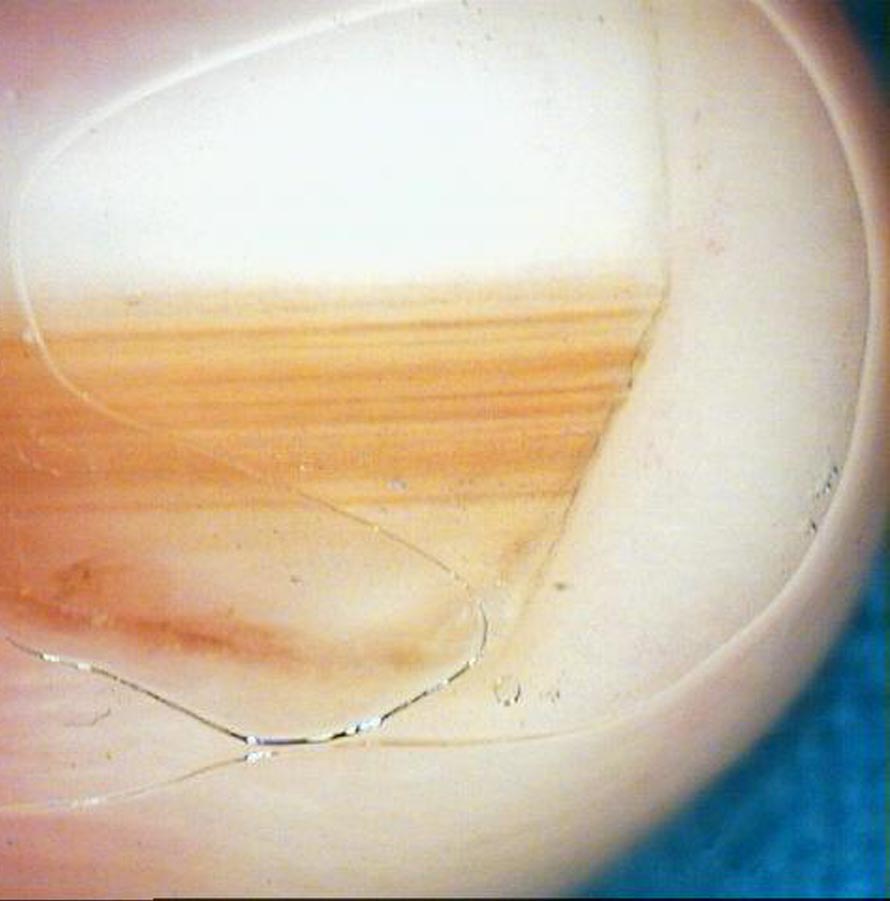
Dermoscopy: Dermoscopy, also known as onychoscopy, is a non-invasive technique that uses a specialized device to examine the nail plate and surrounding structures. It helps differentiate between benign and malignant causes of melanonychia based on specific features, such as melanonychia striata, pigmented bands, or an irregular pigment network.
Digital dermoscopy follow-up: In borderline cases, high-resolution digital dermoscopy photographs can be taken at different time points to evaluate the development of melanonychia over time and distinguish between benign and malignant conditions.
Biopsy: In cases where the diagnosis remains unclear or malignancy is suspected, a biopsy may be recommended. This involves removing a small tissue sample from the nail matrix area for histopathological evaluation. A biopsy helps confirm the diagnosis and determine the presence of malignant cells.
The treatment of melanonychia depends on the underlying cause and the results of diagnostic evaluations. Treatment options may include:
Follow-up: For melanonychia attributed to benign factors like trauma or medication, regular monitoring may be recommended. During follow-up, any changes in size, shape, or color are investigated to ensure the condition remains stable and does not progress, which may require further evaluation.
Treatment of underlying conditions: If melanonychia is secondary to a systemic disease or infection, addressing the primary condition may resolve the nail discoloration. This can involve drug treatment for bacterial or fungal infections, addressing nutritional deficiencies, or managing systemic diseases.
Surgery: In cases where melanoma or other malignant lesions are suspected, surgical intervention may be necessary. This typically involves excising the affected part of the nail matrix or nail bed along with a margin of healthy tissue.
Melanonychia, characterized by nail discoloration, requires a comprehensive approach to diagnosis and management. The evaluation process includes a thorough medical history, physical examination, dermoscopy, digital dermoscopy monitoring, and, if needed, a biopsy. Treatment options range from regular monitoring and addressing underlying conditions to surgical intervention in cases of suspected malignancy. By understanding the diagnosis and management of melanonychia, dermatologists can ensure timely intervention and appropriate treatment for their patients.
If you have located a suspicious lesion on the skin, especially if it is unusual, new or recently changed, contact a dermatologist as soon as possible in order to diagnose the lesion and decide on further treatment.
Give us a call or fill in your details and we will get back to you